The life of a neurosurgeon is surely not a simple, stress-free one, especially when it comes to the removal of an operable brain tumor. As lead investigator, Alfredo Quinones-Hinojosa, MD, professor of neurosurgery, neuroscience and oncology at the Johns Hopkins University School of Medicine, Baltimore, Maryland, says “As a neurosurgeon, I’m in agony when I’m taking out a tumor.”
So many things can go wrong during brain surgery. During the removal of a tumor the surgeon must be aware of the fact that if they do not remove enough of the cancerous tumor, the cancer could eventually return to the patient, but if they take too much the procedure could ultimately kill the patient or leave them permanently disabled.
It can be very difficult for neurosurgeons to differentiate between the tumor cells and normal brain cells, especially along the edge of the tumor, and this has made it challenging for the surgeons to know exactly where to cut. The brain is unlike anywhere else on the body, where extra tissue can be removed safely without further harm to the body. Parts of the tumor must always be left over in order to ensure that the doctors do not remove any healthy brain cells, which could negatively affect the patient’s speech and motor skills.
New technology known as optical coherence tomography (OCT) has allowed for an easier distinction between cancerous tumor cells and healthy brain cells. This has enabled neurosurgeons to remove more of the tumor, thus vastly improving the patient’s chances of complete remission. According to Carmen Kut, a medical student and lead author at Johns Hopkins University School of Medicine, “It has been recently shown that 70% of a brain tumor needs to be removed to have an effect on survival, and survival improves with every extra 5% of the tumor removed. Our results suggest this new technology should enable up to 95% of the tumor to be removed, which could have dramatic effects on survival.”
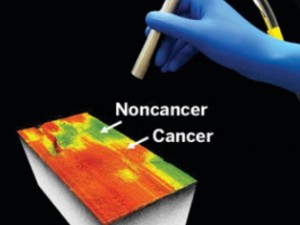
Xingde Li, PhD, professor of biomedical engineering at Johns Hopkins led the group behind the development of this new technology. Li described the technology as working “like ultrasound but uses light instead of sound to give a picture of the tissue.” The way it works is that the surgeon aims the probe at different areas of the tumor, light is then sent passing through and the amount of light absorbed in different areas of the tumor is calculated. The result of calculating the light absorption is known as the optical attenuation coefficient. When the tissue is healthy the light bounces back off the myelin sheath giving a high optical attenuation, but when cancer has infected the brain cells the myelin sheath breaks down with less light reflecting resulting in a much lower optical attenuation. This can help show exactly which parts of the tumor are cancerous and which parts are healthy brain tissue.
This new development in the area of brain cancer will definitely save lives not only in the long term, but also in the very near future.









